– perhaps via direct pudendal nerve stimulation
Earlier in 2017 this paper popped up in JAMA.[1] It was from the same group that had published a huge multicentre trial of electroacupuncture (EA) for chronic severe functional constipation,[2] which was featured in a previous blog. This was a large sham controlled trial (n=504) although not as big as the previous one on constipation (n=1075).
We have known for some time that EA can influence symptoms in overactive bladder, albeit under another name.[3] These are mainly urge symptoms, and a simiar mechanism that reduces pain perception might be postulated to explain the results. Urinary stress incontinence (SUI) seems entirely different, and so the results of this trial were rather unexpected (by me at least).
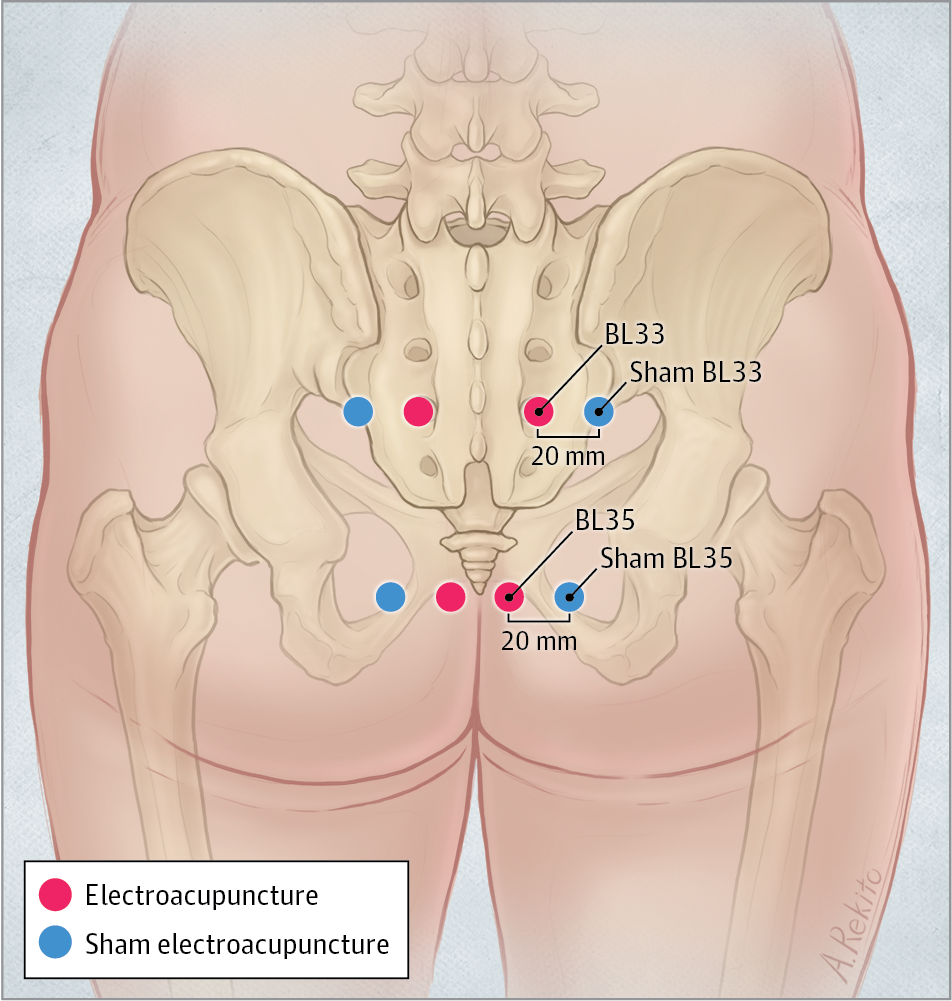
I revisited the paper to examine the intervention in more detail and consider the anatomy involved. The active EA intervention involved just two points on each side (I love the simplicity!) – BL33 and BL35. 75mm needles were employed, and inserted 50 to 60mm. At BL33 the angulation (oblique inferiomedial) aimed to have the needle tip entering the S3 foramina. At BL35 (just lateral to the coccyx) the needle was angled superiolateral. In terms of safety, the structure to be avoided in this area is the rectum, and a paper in Acupuncture in Medicine studied the position of needle tips relative to the rectum when inserted into sacral foramina,[4] but not BL35. Needles inserted into S4 got close to the rectum (4-8mm), but there was a bigger margin in S2 and S3 (19-29.5mm). At BL35, a sufficient lateral angulation would avoid getting close to the rectum, but this angulation would be critical.
Figure 1 from Lui et al JAMA 2017[1]
In terms of physiological effects the needle placement at the S3 foramina would certainly stimulate the dorsal ramus of S3, and possibly the ventral ramus, depending on depth. A superiolateral angulation at BL35 might approach the pudendal nerve as it passes over the sacrospinous ligament, lateral to the sacrum at about the level of S4 (sacral hiatus). Direct stimulation of the pudendal nerve has been described in a small case series of patients with spinal stenosis refractory to less invasive EA,[5] and nerve stimulation was confirmed by perineal sensation. The study in JAMA on SUI does not mention perineal sensation but just mentions mild shivering of the skin around the points, presumably secondary to muscle contraction. EA at 50Hz was applied at a current of 1-5mA. If either needle tip was close to motor fibres, the relevant muscle would have contracted quite strongly for the entire period of stimulation (30 minutes). The authors do not report such effects, but they do discuss the possibility of S3 and pudendal nerve stimulation. If direct electrical nerve stimulation occurred, the effect may have been in some part attributed to pelvic floor muscle contraction induced by motor nerve stimulation. With this in mind it is interesting to note that the effect observed after 18 sessions over 6 weeks was similar to 12 weeks of a pelvic floor exercise programme.
I should note that the sham technique involved no skin penetration and no electrical output, so if there was direct motor nerve stimulation in the active group, there would have been quite a considerable difference in terms of the physiological stimulation applied between the groups.
References
- Liu Z, Liu Y, Xu H, et al. Effect of Electroacupuncture on Urinary Leakage Among Women With Stress Urinary Incontinence: A Randomized Clinical Trial. JAMA 2017;317:2493–501. doi:10.1001/jama.2017.7220
- Liu Z, Yan S, Wu J, et al. Acupuncture for Chronic Severe Functional Constipation: A Randomized Trial. Ann Intern Med 2016;165:761–9. doi:10.7326/M15-3118
- Peters KM, Carrico DJ, Perez-Marrero R a, et al. Randomized Trial of Percutaneous Tibial Nerve Stimulation Versus Sham Efficacy in the Treatment of Overactive Bladder Syndrome: Results From the SUmiT Trial. J Urol 2010;183:1438–43. doi:10.1016/j.juro.2009.12.036
- Katayama Y, Kamibeppu T, Nishii R, et al. CT evaluation of acupuncture needles inserted into sacral foramina. Acupunct Med 2016;34:20–6. doi:10.1136/acupmed-2015-010775
- Inoue M, Hojo T, Nakajima M, et al. Pudendal nerve electroacupuncture for lumbar spinal canal stenosis – a case series. Acupunct Med 2008;26:140–4.pm:18818559
Declaration of interests
I am the salaried medical director of the British Medical Acupuncture Society (BMAS), a membership organisation and charity established to stimulate and promote the use and scientific understanding of acupuncture as part of the practice of medicine for the public benefit.
I am an associate editor for Acupuncture in Medicine.
I have a very modest private income from lecturing outside the UK, royalties from textbooks and a partnership teaching veterinary surgeons in Western veterinary acupuncture. I have no private income from clinical practice in acupuncture. My income is not directly affected by whether or not I recommend the intervention to patients or colleagues, or by whether or not it is recommended in national guidelines.
I have not chaired any NICE guideline development group with undeclared private income directly associated with the interventions under discussion. I have participated in a NICE GDG as an expert advisor discussing acupuncture.
I have used Western medical acupuncture in clinical practice following a chance observation as a medical officer in the Royal Air Force in 1989. My opinions are formed by data that spans the range of quality and reliability, much of which is in the public domain.
I have a logical mistrust of the motives of anyone who advertises an interest or hobby in being a ‘Skeptic’, as opposed to using appropriate scepticism within their primary profession, or indeed organisations that claim to promote generic ‘science’ as opposed to actually engaging in it.