– it seems to work after an intensive course…
About a year ago I was surprised to see a sham controlled RCT of electroacupuncture (EA) published in Annals of Internal Medicine.[1] I was surprised for several reasons: I review for Annals, and I had not seen the paper for review; it was on chronic severe functional constipation – a subject with few previous RCTs of acupuncture; it was positive; it was the biggest 2 arm RCT in the acupuncture literature to date (n=1075).
The treatment was relatively straightforward – EA to the rectus abdominis muscle bilaterally (ST25—SP14) and manual stimulation of a point in tibialis anterior bilaterally (ST37). The sham control involved shallow needling of points close by, but not on the meridians, avoidance of typical needling sensation (de qi) and sham EA (ie no electrical stimulus, but the power indicator and sound as if it were real EA). The frequency used varied from 10 to 50Hz and the intensity was between 0.1 and 1mA. The frequency covers the best range for autonomic modulation (as judged by visceral blood flow), but the intensity was varied from sub-threshold (in terms of nerve stimulation you generally need 0.3 to 0.5mA for the lowest electrical threshold nerves to respond) to a rather gentle stimulus of 1mA. In my experience, many patients do not perceive sensation until around 1.5mA when needle tips are placed into muscle.
Twenty-eight sessions were provided over 8 weeks – 5 sessions per week for the first 2 weeks, and 3 sessions per week for the next 5 weeks. So it was quite an intense course of treatment. There was no comment about rotation of needling sites – with such an intense treatment regime it is common to alternate similar protocols so that needle sites do not get sore.
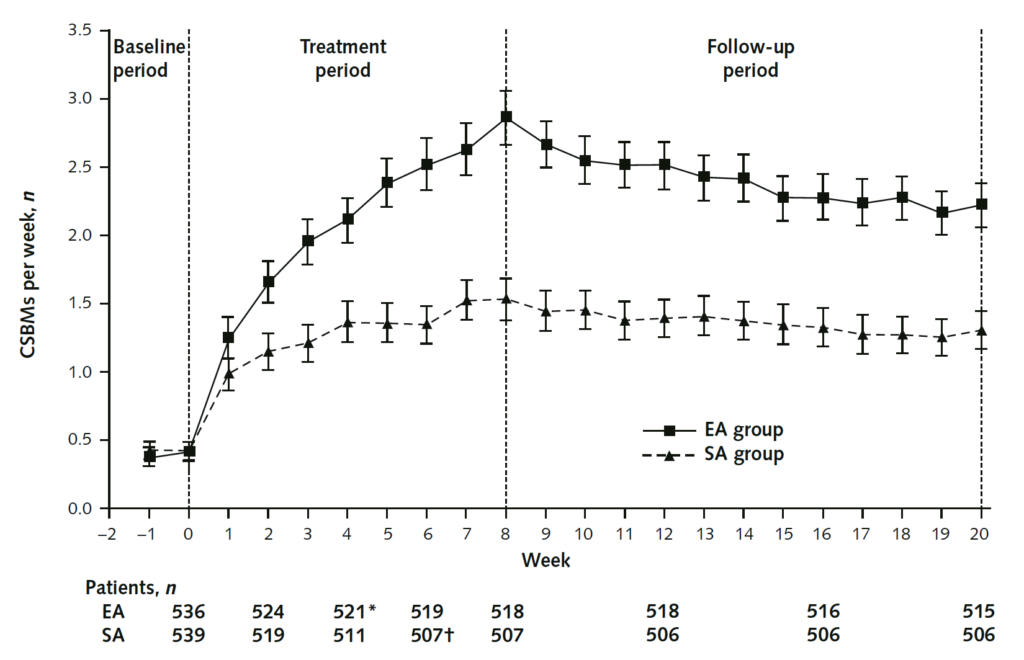
The primary outcome was based on a stool diary and was the number of complete spontaneous bowel movements (CSBM) per week. EA performed significantly better than sham at 8 weeks and the effect was maintained at 12 weeks follow-up.
Figure 2 from Lui et al Ann Int Med 2016[1]
Blinding appears to have been maintained at 4 and 8 weeks from a random sample of 140 participants. At 8 weeks about 90% from each group guessed that they had received the real EA.
The size of the effect appears to be clinically relevant, with a change from baseline in CSBM of greater than 1 per week,[2] although the group average does not exceed 3 per week so most participants in the active group would still be considered to have constipation.
Of interest is a follow-up paper published recently that examines factors associated with the response to acupuncture in this trial. It found that age was inversely related to response to acupuncture (ie younger patients did better), and comorbidities reduced the likelihood of response.[3]
References
- Liu Z, Yan S, Wu J, et al. Acupuncture for Chronic Severe Functional Constipation: A Randomized Trial. Ann Intern Med 2016;165:761–9. doi:10.7326/M15-3118
- Johanson JF, Wald A, Tougas G, et al. Effect of tegaserod in chronic constipation: a randomized, double-blind, controlled trial. Clin Gastroenterol Hepatol 2004;2:796–805. doi:10.1016/S1542-3565(04)00356-8
- Yang X, Liu Y, Liu B, et al. Factors related to acupuncture response in patients with chronic severe functional constipation: Secondary analysis of a randomized controlled trial. PLoS One 2017;12:e0187723. doi:10.1371/journal.pone.0187723
Declaration of interests
I am the salaried medical director of the British Medical Acupuncture Society (BMAS), a membership organisation and charity established to stimulate and promote the use and scientific understanding of acupuncture as part of the practice of medicine for the public benefit.
I am an associate editor for Acupuncture in Medicine.
I have a very modest private income from lecturing outside the UK, royalties from textbooks and a partnership teaching veterinary surgeons in Western veterinary acupuncture. I have no private income from clinical practice in acupuncture. My income is not directly affected by whether or not I recommend the intervention to patients or colleagues, or by whether or not it is recommended in national guidelines.
I have not chaired any NICE guideline development group with undeclared private income directly associated with the interventions under discussion. I have participated in a NICE GDG as an expert advisor discussing acupuncture.
I have used Western medical acupuncture in clinical practice following a chance observation as a medical officer in the Royal Air Force in 1989. My opinions are formed by data that spans the range of quality and reliability, much of which is in the public domain.
I have a logical mistrust of the motives of anyone who advertises an interest or hobby in being a ‘Skeptic’, as opposed to using appropriate scepticism within their primary profession, or indeed organisations that claim to promote generic ‘science’ as opposed to actually engaging in it.