This piece has also been stimulated by a publication in JAMA, this time evaluating the use of denervation of joints in spinal pain.[1] It is a set of three large (n=251, n=228, n=202), probably definitive, pragmatic trials that evaluate the use of radiofrequency denervation (RFD) as an addition to a 3 month standardised exercise programme. The design is such that the intervention was given the greatest possible opportunity to demonstrate an effect, that is both the specific effect of the intervention plus the context in which it is provided. This is rather similar to the Acupuncture in Routine Care (ARC) trials performed as part of the German Modellvorhaben Akupunktur;[2] all of which were markedly positive for acupuncture.
The results seem clear – at no time point did the difference been intervention and control reach clinical significance in terms of pain intensity (the primary outcome); and in only one of 18 time points across the three trials did the difference reach statistical significance (the 3 week outcome in the sacroiliac joint trial). The measure used for clinical significance here was 2 points on a 0-10 scale of pain, or 20mm on a 100mm visual analogue scale, but at no point did RFD achieve the lower level of 1 point set by NICE in NG59.[3]
The data from NG59 comparing acupuncture with no acupuncture controls (the closest equivalent comparison to the current trials of RFD) gave a pooled result at less than 4 months of more than 60% greater than the best outcome recorded in these trials of RFD. A result that was both statistically significant and clinically relevant by the standards used in NG59, although it would not have reached the standard set in these trials.
So what is RFD, and why am I drawing attention to this? RFD is a method of burning nerves, and the idea is that by denervating a pain source in the spine you might achieve sustained pain relief in chronic back pain. The typical targets are facet joints, sacroiliac joints and intervertebral joints. The radiofrequency term is unnecessarily confusing since the method uses electrical pulses at about 5000Hz rather than electromagnetic radiation in the radiowave spectrum. The latter stretches roughly from 3×103Hz to 3×109Hz equating respectively to wavelengths from 100km to 1mm, but that’s enough physics for now. Basically the high frequency electrical pulses cause a heating effect at the tip of the RFD probe and it typically reaches 80 degrees C, which coagulates the tissues at the tip.
Isn’t burning nerves a bit of an archaic technique? Yes it is, and in principle modern pain medicine tends to try to avoid neurolytic treatments. Damaging nerves can cause neuropathic pain in some individuals, and the nerves can grow back anyway.
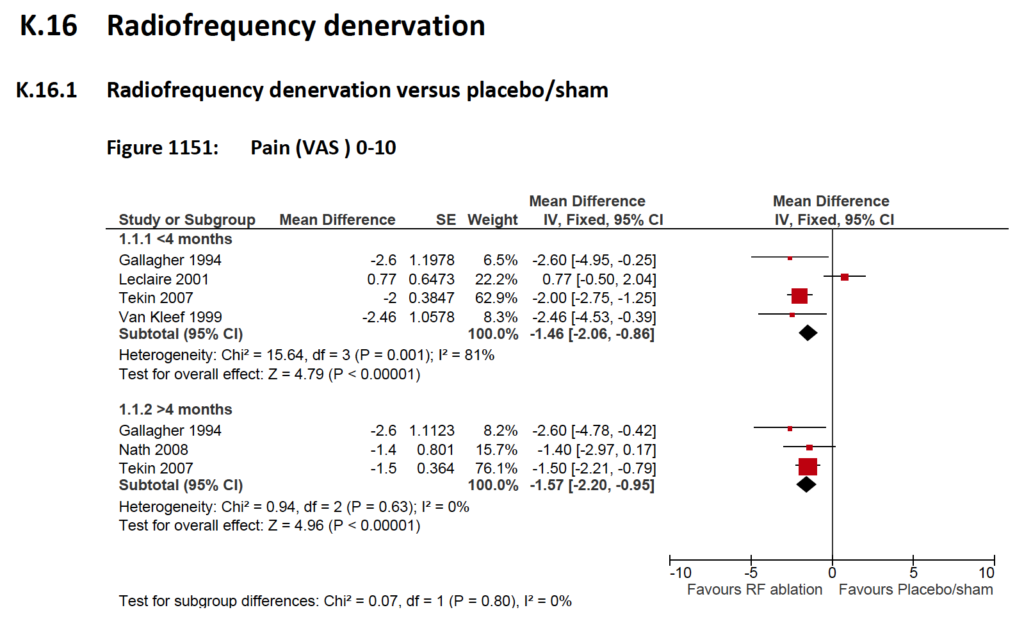
Why was it recommended in NG59? This decision was controversial because the guideline development group (GDG) for NG59 recommended RFD based on quite limited data from very small trials, and the current Cochrane review clearly concluded that the evidence was insufficient to recommend it.[4] The decision to recommend RFD and recommend against acupuncture was also controversial because of potential conflicts of interests of interventionists on the GDG and how these were addressed.[5]
In reviewing the data on RFD used by NG59, I discovered that there was quite disproportionate weighting given to one particular trial despite it only having 20 patients per group (Tekin 2007 [6]). The reason for this is the meta-analytic software favours trials with low standard errors.
K.16.1 from Appendices K-Q of NG59
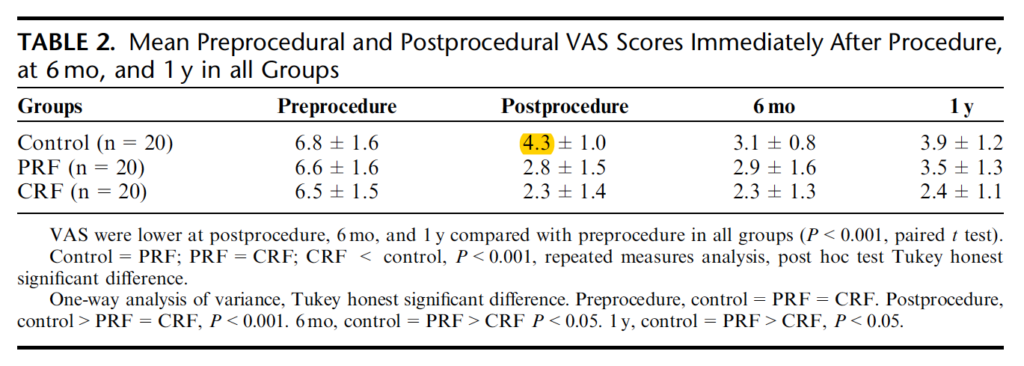
Anyway, I thought I would take a closer look at this paper, and discovered that the control group dropped from 6.8 to 4.3 on a 0 to 10 pain score from pre- to post-procedure. The slightly funny thing about this was that the control procedure involved exactly the same intervention as was used to determine eligibility for the trial – a diagnostic medial branch block ie a local anaesthetic block to the nerve that would then be coagulated or burnt in the active (CRF) group. In order to get in the trial the patients had to have a reduction in pain score of 50% or more, yet the control group who went on to have the same procedure again only dropped by about 37% (see Table 2 from Tekin 2007 below).
Table 2 from Tekin 2007
Well it all just goes to show that small trials are unreliable, but what should we do now? We should ask the centre that conducted the guideline (the National Guideline Centre hosted by the RCP) to perform an urgent review on the grounds of safety. As it stands NG59 has all but stopped NHS acupuncture for back pain and is likely to result in a vast increase in the use of RFD, which now we see doesn’t actually do anything worthwhile for patients, but may boost the Maserati-purchasing power of certain interventionists.
References
1. Juch JNS, Maas ET, Ostelo RWJG, et al. Effect of Radiofrequency Denervation on Pain Intensity Among Patients With Chronic Low Back Pain: The Mint Randomized Clinical Trials. JAMA 2017;318:68–81. doi:10.1001/jama.2017.7918
2. Cummings M. Modellvorhaben Akupunktur–a summary of the ART, ARC and GERAC trials. Acupunct Med 2009;27:26–30. doi:10.1136/aim.2008.000281
3. NICE guideline on low back pain and sciatica in over 16s: assessment and management. https://www.nice.org.uk/guidance/ng59. 2016.
4. Maas ET, Ostelo RWJG, Niemisto L, et al. Radiofrequency denervation for chronic low back pain. Cochrane database Syst Rev 2015: CD008572. doi:10.1002/14651858.CD008572.pub2
5. Cummings M. NG59 used different levels of evidence for conventional interventions compared with those for acupuncture and may not have adequately addressed personal financial COIs of the GDG chair. BMJ. 2017;356. http://www.bmj.com/content/356/bmj.i6748/rr-6
6. Tekin I, Mirzai H, Ok G, et al. A comparison of conventional and pulsed radiofrequency denervation in the treatment of chronic facet joint pain. Clin J Pain;23:524–9. doi:10.1097/AJP.0b013e318074c99c
Declaration of interests
I am the salaried medical director of the British Medical Acupuncture Society (BMAS), a membership organisation and charity established to stimulate and promote the use and scientific understanding of acupuncture as part of the practice of medicine for the public benefit.
I am an associate editor for Acupuncture in Medicine.
I have a very modest private income from lecturing outside the UK, royalties from textbooks and a partnership teaching veterinary surgeons in Western veterinary acupuncture. I have no private income from clinical practice in acupuncture. My income is not directly affected by whether or not I recommend the intervention to patients or colleagues, or by whether or not it is recommended in national guidelines.
I have not chaired any NICE guideline development group with undeclared private income directly associated with the interventions under discussion. I have participated in a NICE GDG as an expert advisor discussing acupuncture.
I have used Western medical acupuncture in clinical practice following a chance observation as a medical officer in the Royal Air Force in 1989. My opinions are formed by data that spans the range of quality and reliability, much of which is in the public domain.
I have a logical mistrust of the motives of anyone who advertises an interest or hobby in being a ‘Skeptic’, as opposed to using appropriate scepticism within their primary profession, or indeed organisations that claim to promote generic ‘science’ as opposed to actually engaging in it.