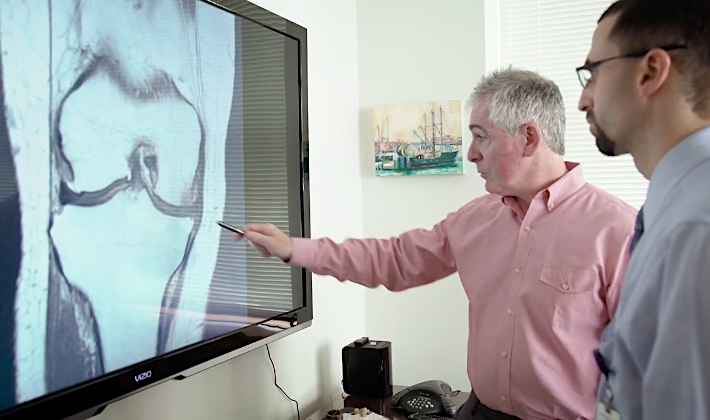
This piece has been stimulated by a recent publication in JAMA evaluating the use of regular intra-articular corticosteroid injections for symptom management and cartilage volume in osteoarthritis (OA) of the knee.[1] Previous research had suggested that the inflammatory process in the knee was associated with both pain and progression of cartilage loss, however, this trial clearly demonstrated a greater loss of cartilage after two years of 3 monthly intra-articular triamcinolone injections compared with the same frequency of saline injections.
It seems pretty clear then that we should avoid long-term use of intra-articular steroid within the knee and probably other synovial joints. Previous research, also published in JAMA, indicates that steroid can also have a negative impact in the long term on lateral epicondylalgia.[2] Furthermore, a systematic review of the effects of local corticosteroid on tendon clearly concluded that the impact was negative both in vitro and in vivo.[3]
In shoulder pain it does not seem to matter whether or not the steroid is injected into the presumed target based on imaging, or whether it is injected into the buttock.[4] Moreover, given the anatomical vulnerability of the human supraspinatus tendon and its propensity for self destruction with age,[5] combined with the known negative effects of steroid on tendon, it looks as though we should avoid steroid in the shoulder too.
So what do we do if we do not inject steroid into our peripheral sources of musculoskeletal pain? We can try injecting other things I guess. Diclofenac, botulinum toxin or maybe normal saline – the latter seems to do very well when used as a control procedure in trials, in terms of the change from baseline. Having been brought up to accept steroid injection as a standard conventional procedure, it was a major surprise to find that needles alone (dry needling or local acupuncture) in tender muscle appeared to be highly effective.[6] Having got over this surprise I was guided through the process of my first systematic review to find that virtually none of the trials of needling and injection therapies in myofascial trigger point pain demonstrated superiority for any individual technique.[7] Indeed, saline injection (the intended control procedure) proved superior in most outcomes of one particularly good quality trial.[8]
Despite saline injection being no less effective in terms of pain relief than an ‘active’ comparator, and being associated with clinically meaningful changes from baseline in trials, we do not use it in practice. Well it has not been tested in a double blind randomised controlled trial… but what would we use in the control group of such a trial? Perhaps the needle without an injection. Then we have the challenge of blinding the practitioner, and we are getting closer to the dilemma of acupuncture research.
Acupuncture needles are less traumatic than hypodermic needles, and carry no risk related to the injected substance. They also carry less from the outside of the organism (skin flora and contaminants) into the internal environment because they lack the hollow bore of a needle for injection. In general we avoid needling into joint spaces with acupuncture needles despite the reduced theoretical risk of carrying in bugs from the outside. The best quality evidence for acupuncture in chronic pain related to osteoarthritis demonstrates and effect size (standardised mean difference) of 0.26 over sham acupuncture (minimal needling in the biggest trials) and an effect size of 0.57 over no acupuncture controls (waiting list, usual care, or guideline-based conventional care).[9] For comparison, topical non-steroidal anti-inflammatory drugs have an effect size of 0.4 over placebo and oral preparations range from 0.29 to 0.44.[10] So 0.57 looks pretty good if you don’t mind buying a bit of the relatively safe context of acupuncture, or if you prefer something more potent you might go for oral opiates which come in at 0.78… but we all know the path from there on, and it does not look so rosey.
Well I would go for the needles, probably with a little umph added from electrical impulses as Jorge Vas did in 2004,[11] with an effect size of 1.21 (this was an outlier in the Vickers IPDM,[9] but the only trial to use electroacupuncture (EA) to muscles around the knee compared with non-penetrating sham EA).
References
1. McAlindon TE, LaValley MP, Harvey WF, et al. Effect of Intra-articular Triamcinolone vs Saline on Knee Cartilage Volume and Pain in Patients With Knee Osteoarthritis: A Randomized Clinical Trial. JAMA 2017;317:1967–75. doi:10.1001/jama.2017.5283
2. Coombes BK, Bisset L, Brooks P, et al. Effect of corticosteroid injection, physiotherapy, or both on clinical outcomes in patients with unilateral lateral epicondylalgia: a randomized controlled trial. JAMA 2013;309:461–9. doi:10.1001/jama.2013.129
3. Dean BJF, Lostis E, Oakley T, et al. The risks and benefits of glucocorticoid treatment for tendinopathy: a systematic review of the effects of local glucocorticoid on tendon. Semin Arthritis Rheum 2014;43:570–6. doi:10.1016/j.semarthrit.2013.08.006
4. Ekeberg OM, Bautz-Holter E, Tveitå EK, et al. Subacromial ultrasound guided or systemic steroid injection for rotator cuff disease: randomised double blind study. BMJ 2009;338:a3112. doi:10.1136/bmj.a3112
5. Vincent K, Leboeuf-Yde C, Gagey O. Are degenerative rotator cuff disorders a cause of shoulder pain? Comparison of prevalence of degenerative rotator cuff disease to prevalence of nontraumatic shoulder pain through three systematic and critical reviews. J shoulder Elb Surg 2017;26:766–73. doi:10.1016/j.jse.2016.09.060
6. Cummings TM. A computerised audit of acupuncture in two populations: civilian and forces. Acupunct Med 1996;14:37–9. doi:10.1136/aim.14.1.37
7. Cummings TM, White AR. Needling therapies in the management of myofascial trigger point pain: a systematic review. Arch Phys Med Rehabil 2001;82:986–92. doi:10.1053/apmr.2001.24023
8. Frost FA, Jessen B, Siggaard-Andersen J. A control, double-blind comparison of mepivacaine injection versus saline injection for myofascial pain. Lancet 1980;1:499–500.pm:0006102230
9. Vickers AJ, Cronin AM, Maschino AC, et al. Acupuncture for chronic pain: individual patient data meta-analysis. Arch Intern Med 2012;172:1444–53. doi:10.1001/archinternmed.2012.3654
10. Birch S, Lee MS, Robinson N, et al. The U.K. NICE 2014 Guidelines for Osteoarthritis of the Knee: Lessons Learned in a Narrative Review Addressing Inadvertent Limitations and Bias. J Altern Complement Med 2017;23:242–6. doi:10.1089/acm.2016.0385
11. Vas J, Mendez C, Perea-Milla E, et al. Acupuncture as a complementary therapy to the pharmacological treatment of osteoarthritis of the knee: randomised controlled trial. BMJ 2004;329:1216.pm:15494348
Declaration of interests
I am the salaried medical director of the British Medical Acupuncture Society (BMAS), a membership organisation and charity established to stimulate and promote the use and scientific understanding of acupuncture as part of the practice of medicine for the public benefit.
I am an associate editor for Acupuncture in Medicine.
I have a very modest private income from lecturing outside the UK, royalties from textbooks and a partnership teaching veterinary surgeons in Western veterinary acupuncture. I have no private income from clinical practice in acupuncture. My income is not directly affected by whether or not I recommend the intervention to patients or colleagues, or by whether or not it is recommended in national guidelines.
I have not chaired any NICE guideline development group with undeclared private income directly associated with the interventions under discussion. I have participated in a NICE GDG as an expert advisor discussing acupuncture.
I have used Western medical acupuncture in clinical practice following a chance observation as a medical officer in the Royal Air Force in 1989. My opinions are formed by data that spans the range of quality and reliability, much of which is in the public domain.
I have a logical mistrust of the motives of anyone who advertises an interest or hobby in being a ‘Skeptic’, as opposed to using appropriate scepticism within their primary profession, or indeed organisations that claim to promote generic ‘science’ as opposed to actually engaging in it.