 India reports more cases of tuberculosis than any other country. This much is well known. However, nobody quite knows the true magnitude of the TB problem in the country.
India reports more cases of tuberculosis than any other country. This much is well known. However, nobody quite knows the true magnitude of the TB problem in the country.
For one, we do not know the number of TB patients who do not seek care or who remain undiagnosed, but we refer to this often as the “missing million.” Also, until recently, we did not have the foggiest idea of the number of TB patients treated in India’s vast, fragmented private sector. Currently, many private providers and hospitals do not notify the government of TB cases, despite TB being made a notifiable disease in 2012.
This can change. There is now a significant opportunity to scale up systems for private providers to notify TB cases; for TB patients to benefit from free, essential services; and for the government to correctly count all public and private TB cases so we can know how well disease control is working—creating a win-win situation for all.
A series of studies that we contributed to, published in The Lancet Infectious Diseases, provide several new insights into TB in the private sector, and might help direct strategies for tackling TB. In the first study, the researchers took advantage of a unique data window into the private sector: a large, national database on the sales and distribution of anti-tuberculosis drugs in the private sector. The analysis suggested that 2.2 million cases could plausibly have been treated in the private sector in 2014 alone—more than double the number suggested by previous estimates. This shows the sheer scale of the effort that will be required to reach private providers, and to attract notifications for privately treated TB patients.
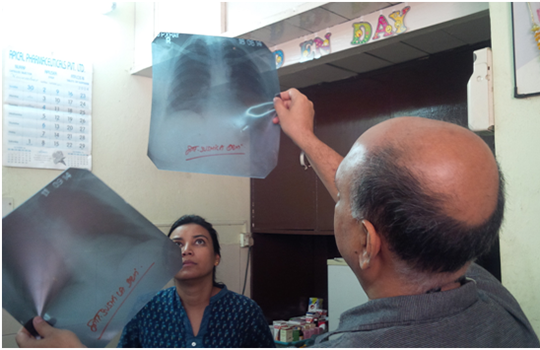
The other studies provided useful insights into who exactly was prescribing these enormous quantities of TB medicines. Here, the researchers used simulated patients, presenting with classic TB symptoms or documented evidence of TB disease, to assess what various providers actually did when faced with such patients. The results of these studies clearly showed that—at least in urban areas—allopathic private doctors are treating TB.
Reassuringly, informal and AYUSH practitioners rarely dispensed anti-tuberculosis drugs and pharmacists never dispensed them over the counter. However, these providers rarely tested for TB even when patients presented with typical symptoms or abnormal chest x-rays. Thus, while they may not be misusing TB drugs, they may be contributing to delays in TB diagnosis by using other antibiotics and non-specific therapies.
These studies come at a time when India’s Revised National TB Control Program (RNTCP) and state and city governments have succeeded in demonstrating innovative, workable, and scalable solutions. In several settings, the RNTCP has effectively engaged private providers, successfully attracting large numbers of private TB case notifications. With that information, the RNTCP has improved the diagnosis of patients with free tests, provided patients with free TB drugs, and extended adherence support to increase rates of TB treatment completion.
These innovative approaches are bringing previously invisible, privately treated TB patients into the light of public health services, where care and adherence can be monitored. Thanks to the information and communications technologies deployed, these projects are also generating unprecedented data on TB outcomes in the private sector.
Private providers engaged in these projects are seeing the value their TB patients are getting through free test vouchers, free TB drugs, and continuous support and counselling to ensure treatment completion. This value, in turn, helps them retain their patients, secure their respect, and grow their practice. Private practitioners also appreciate the direct human contact they have with public health workers, getting feedback on how their patients are progressing, and helping their patients sustain a full course of treatment. Most importantly, they appreciate being made a partner in their city’s TB control effort.
To scale up these effective interventions to reach all TB patients, it is critical for the government to take TB control as a genuine mission and to make serious financial investments. Simply put, treating twice as many TB patients will cost twice as much budget as is currently being provided, and that should be a fantastic investment for the nation because TB control is a very cost effective strategy with exceptional return on investment from a societal perspective. From an economic perspective, investing in the Global Plan to End TB is estimated to deliver India $364 billion as overall economic return. Any plan to end TB in India must include a comprehensive approach to partnering with the private sector. Otherwise, more than half of the TB burden in the country will be left unaddressed.
Equally importantly, TB patients cannot remain invisible. There is a need for more robust estimates of the TB burden and continued efforts to measure quality of care in the private sector. Countries such as China have made serious investments in TB control, effectively used repeated rounds of national TB prevalence surveys to track their TB epidemic, and have shown major reductions in prevalence over time. India needs to do the same, and we applaud the direct disease burden estimation that RNTCP has proposed via a national TB prevalence survey.
Yet prevalence estimation is not enough; the TB programme needs to track and support individuals with TB. The RNTCP’s Nikshay TB case notification system offers hope that case notifications can result in meaningful public health action. This will require investment in information and communications technologies infrastructure and real time data intelligence.
Lastly, leadership is critical and India is starting to step up. The Indian government has taken several steps over the past few years to address TB. This includes making TB a notifiable disease, developing the Standards for TB Care in India, introducing daily drug regimens, and rolling out molecular and drug susceptibility testing.
Yet there is an opportunity to do more and better, and for India to assume a global leadership role. With its strong research expertise in TB, biotech and IT capacity, and recent successes (for example, polio elimination; indigenous rotavirus vaccine), India has the potential to lead from the front. With strong financial and political commitment from Prime Minister Modi and his cabinet, India can take on tuberculosis.
Madhukar Pai is a Canada research chair in epidemiology & global health at McGill University, Montreal, where he directs Global Health Programs. Twitter: @paimadhu
Nimalan Arinaminpathy is a senior lecturer in the Department of Infectious Disease Epidemiology, in the School of Public Health, at Imperial College, London.
Authors’ competing interests: None declared.
This blog was first published on www.scroll.in website.