![]() What can we do to improve care for people who are dying? Someone dies every minute in the UK. In healthcare we know we need to improve what we are doing, but the messages in guidelines and strategies have changed little over recent years.
What can we do to improve care for people who are dying? Someone dies every minute in the UK. In healthcare we know we need to improve what we are doing, but the messages in guidelines and strategies have changed little over recent years.
Public health agendas in palliative and end of life care are increasingly promoted to empower people to have conversations about the end of life, death, and dying, with the philosophy that “care for one another at times of crisis and loss is not simply a task for health and social care services, but is everyone’s responsibility.”
GPs are considered to be embedded in their communities and should therefore be in a prime position to engage in these public health agendas. As a GP in busy Birmingham, I find managing the necessary conversations about deteriorating health conditions and end of life care ever more difficult due to conflicting demands on time, and I am not alone. Yet this is a vital part of our role as GPs. Breaking down the social barriers to these conversations and empowering people to voice their preferences could really help. Over the past two years I have become involved in a project that aims to do just that.
It started in 2015, with a small group of motivated people who organised a marketplace event during Dying Matters Awareness week, with undertakers, florists, nurses and doctors, hospice providers, artists, and celebrants.
Since then, the group has been growing as a true (voluntary) community collective, now called “BrumYODO” (YODO—You Only Die Once). The aim of BrumYODO is to help the people of Birmingham have more open and honest conversations about death and dying. This year BrumYODO organised and promoted a full programme of Dying Matters Awareness Week events across Birmingham.
The programme was launched at Kings Heath Farmers Market on Saturday 7 May. Then there was a “pop-up shop” in Kings Heath for the week, hosting a range of events including coffin decorating and opportunities to meet hospice teams, Macmillan nurses, will writers, and solicitors. There was a shroud demonstration; an “Ask the Undertaker” session; and an interview conducted by the philosopher Nigel Warburton with Dr Ros Taylor MBE, “The Philosophy of Choice in the Face of Death.”



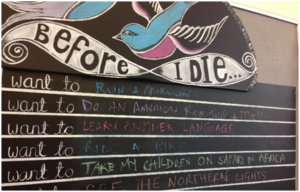
“Death Cafés” were held every day in coffee shops across Birmingham and “Before I Die Walls” appeared in libraries, hospitals, high streets, and bus stops. There were also book displays at local libraries, hospice information days, a story telling night, and a bus trip to a natural burial ground. The week was brought to a close with a “Death Disco.”

We had a website, a Twitter account (@BrumYODO), and a Facebook page; articles in community magazines and in the Birmingham Mail. BrumYODO was on local radio and featured as the Academy of Fabulous Stuff NHS “pick of the week.” The 2016 BrumYODO film was “premiered” on 12 July to a diverse audience of people from all over Birmingham.
Finding the time to engage in a project like BrumYODO around work is a challenge. The tradeoff is how exciting it is to be involved in a community project, witnessing this wider and much needed recognition of the multiple losses associated with incurable conditions, dying, and bereavement. I hope that by raising awareness in this way, more people will take control of conversations, which have become increasingly medicalised over recent decades, and begin talking openly to their healthcare providers about their preferences. Our challenge now is to keep the conversation going and hope that it leads to benefits for everyone.
Sarah Mitchell is a GP in Birmingham and NIHR doctoral research fellow at the University of Warwick. This blog is presented on behalf of the BrumYODO Collective.
Competing interests: I have read and understood BMJ policy on declaration of interests and declare no competing interests.