There is something different about medics. We stand out at university – often forming into a clique that others find difficult to fathom, break into, or tolerate. We strive to be different in many ways; we learn a huge range of facts and figures, along with new languages ( we are taught about everything from the arachnoid mater to xanthelasma, via dysdiadochokinesia) and new ways of behaving – “Hello, my name is…. I’d like to examine your chest if I may?”
This difference has been reinforced over centuries, helped along by the formation of royal colleges, and more recently, by real successes in actually curing some diseases, and managing others so that hospitals are no longer feared as places of death, but instead as places of relative safety for those needing their services.
I think that this paper in the January edition of the PMJ may help to take us back to our roots a little. The paper is a quality improvement report looking at the impact of a mnemonic device on the completeness of information recorded in the notes in a paediatric department. The problem was that documentation was of a poor standard, impairing the investigation of complaints and incidents. The solution used an acrostic to help junior doctors record the important aspects of care that are encompassed within the post-take round.
Results were impressive, showing an increase in completeness of the notes in areas that were previously neglected, including parental concerns, fluid prescriptions, nursing concerns, and investigations. Understandably there was less increase in areas that had been previously well documented – the final plan, vital signs, presenting problems, and examination findings.
So we can see that, in a time-pressured, complex situation, the junior members of a team find that they are better able to record relevant information when following a set pattern of information recall / record for each case. This is not perhaps a Nobel-worthy discovery, but it is an important contribution to the ongoing realisation in our profession that there are tools and techniques we can use to enhance our practice, and improve safety and outcomes of the processes we use in our daily work.
Many of the ‘new’ ideas in healthcare like LEAN, six sigma, crisis resource management, human factors training, pitstop handovers, checklists and so on have origins outside of medicine, and in other high-risk, high-reliability, or high value organisations. The impact of these ideas though can be significant, and in some cases hospitals have been impressed enough to adopt philosophies from industry wholesale – notably the Royal Bolton Hospital. The medical profession itself though is usually somewhat more reluctant to adopt these concepts, and apply them in practice.
The resistance to checklists, communication methods like SBAR, and other tools that seem to constrain clinical autonomy provides an interesting point to consider. Is there something inherently wrong in encouraging medics to communicate or work in standardised ways?
Well, no. The ALS algorithm – much maligned by those who have to repeatedly take assessments and refresher courses using the same stock phrases, and act out scenarios that have an uncanny knack of ending in a cardiac arrest – has had great success. Indeed, when you think of the teams that work in any hospital, the arrest team is one of the most efficient in terms of understanding common purpose, using a common language, and following a set pattern of actions. This process even works across language barriers as Dr Davies showed in this article.
And yet, there is always something uncomfortable about being asked to write / think / talk / communicate in a particular way as a medic. Is this because we are somehow different from those other human beings working in complex, challenging environments?
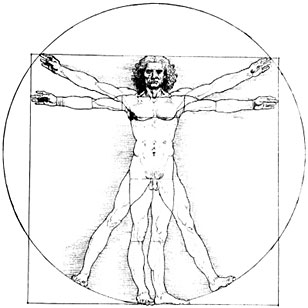
My feeling is that perhaps we aren’t entirely to blame for our reluctance to adopt these ‘new’ ideas of working. The hubris required to enter chaotic, painful, emotional situations, take control, decide on a decisive course of action, and do this within a very short space of time is bred into us from the point at which we decided to become doctors. As I said at the start – we medics are different – and have been since we started on our journey to the positions we now hold.
And therein lies the rub. When it comes down to it, we aren’t really different from those we try to guide through the challenges of illnesses both acute, long-term and terminal. We have the same brains, same cognitive biases and same susceptibility to distraction, and therefore next time you are asked if you can follow an acrostic, use a checklist, or submit to a protocol – before rejecting the concepts out of hand, consider if you are doing so because the tool really isn’t fit for the job, or if you need to follow the advice of Naomi Campbell – don’t believe your own hype.