By James Griffiths, Consultant in Emergency Medicine, Barnsley Hospital NHS Foundation Trust
Background
Occult scaphoid fracture (clinical signs of fracture but normal initial plain X-ray) is a common presentation to emergency departments and there is a lack of consensus in the literature with regard to management, in particular, second-line imaging. The Royal College of Radiologists recommends magnetic resonance imaging (MRI) as the second line approach, with bone scintigraphy and computed tomography (CT) as alternatives[1].
A survey of UK orthopaedic trainees revealed a wide variation in the management of occult scaphoid fractures and suggested standardising their management to ensure early diagnosis and limit unnecessary wrist immobilisation[2]. However, as many UK emergency departments will not refer these patients on to orthopaedics until the fracture is confirmed, it is important to ascertain how these patients are currently being managed outside of fracture or orthopaedic clinics in the UK.
A survey of Australian directors of emergency medicine training also revealed variation in practice and that the vast majority of sites (83%) did not have a guideline or protocol for occult scaphoid fracture[3].
Methods
A 1-page questionnaire was written (see online appendix) and sent to the clinical lead in 237 UK emergency departments. Of particular interest was whether occult scaphoid fractures are followed up in ED or fracture clinic; what time frame patients are reviewed in; what second line imaging is used, and what form of immobilisation is carried out.
A total of 153 responses were received, giving a response rate of 65%.
58% of responders are currently managing occult scaphoid fractures in emergency department returns clinic and 73% of departments currently have a protocol for occult scaphoid fracture.
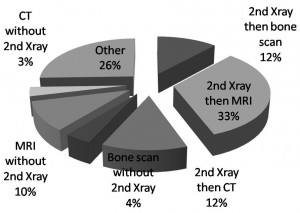
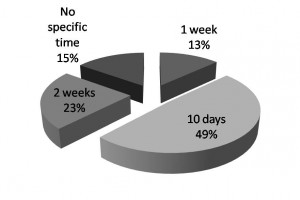
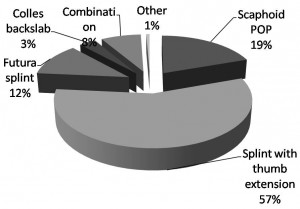
As can be seen from figures 1-3, there is a wide variation in UK ED practice in terms of: timing of follow-up, second line imaging and method of immobilisation.
Discussion
The management of occult scaphoid fractures remains problematic for both emergency departments and colleagues in orthopaedics. In cases of inadequate or delayed diagnosis, possible problems in union can lead to functional wrist problems[4] However, unnecessary immobilisation and imaging has costs for the patient, hospital and society[5]. It is estimated that the fear of under-treatment results in over-treatment of five out of six patients[6].
What this survey of UK emergency departments shows, is that, in common with previous surveys[2,3], there is wide variation in the management of occult scaphoid fractures. Hopefully the forthcoming Cochrane review[7] will provide guidance at least in terms of second-line imaging, so that UK practice can be standardised. This will enable physicians to reduce unnecessary immobilisation without increasing the risk of non-union or avascular necrosis.
Conclusion
Over half of UK EDs currently manage occult scaphoid fractures in their ED clinic and the majority currently have a protocol within the department. However, there is wide variation in practice with regard to both second line imaging and method of immobilisation.
Acknowledgements
I would like to thank all the respondents who took the time to complete and return the survey.
References
- Baldassarre RL, Hughes TH. Investigating suspected scaphoid fracture. BMJ 2013;346:f1370
- Brookes – Fazakerley SD, Shyam Kumar AJ, Oakley J. Survey of the initial management and imaging protocols for occult scaphoid fractures in UK hospitals. Skeletal Radiol 2009;38:1045-1048
- Kelly AM. Initial management of potential occult scaphoid fracture in Australasia. Int J Emerg Med 2010;3:45-47
- Rhemrev SJ, Ootes D, Beeres FJ et al.Current methods of diagnosis and treatment of scaphoid fractures. Int J Emerg Med 2011;4:1-8
- Patel NK, Davies N, Mirza Z et al. Cost and clinical effectiveness of MRI in occult scaphoid fractures: a randomised controlled trial. Emerg Med J 2013;30:3 202-207
- Mallee W, Doornberg JN, Ring D et al. Comparison of CT and MRI for diagnosis of suspected scaphoid fractures. J Bone Joint Surg Am 2011;93(1):20-28
- Malle WH, Doornberg JN, Poolman RW et al. Computed tomography versus magnetic resonance imaging versus bone scintigraphy for clinically suspected scaphoid fractures in patients with negative plain radiographs. Cochrane Database of Systematic Reviews 2012, Issue 8.Art. No.:CD010023