Sport and Exercise Medicine: The UK trainee perspective (A twice-monthly series on the BJSM blog)
By Dr James Noake
Most of the clinicians reading this blog currently possess or have previously had a sporting pedigree of some description. I would predict that a large number of you would state that this is what brought you into the SEM sphere in the first place. With sporting participation there inevitably looms the spectre of injury. We’ve swapped harrowing tales about our misfortunes on the field of play and the subsequent gruesome surgical interventions, vying for VAS one-upmanship. I am no exception – my post-operative comeback was more lame duck than ‘phoenix from the flames’.
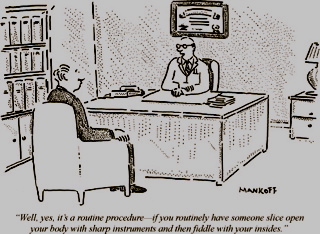
So when presented with a patient in clinic with a similar injury to ours, what do we find ourselves advising them? Can we hand-on-heart declare that we assess the clinical situation 100% objectively without introducing bias derived from our own experiences – negative or positive? As clinicians, we are in a privileged position with unparalleled influence on our patients’ decisions about their own illness or injury. We are traditionally taught to strive for empathy as the benchmark for communication skills, and clearly it is important for upholding the doctor-patient relationship. Having a personal perspective on the sports injury bestows the SEM clinician with genuine insight, which can rescue even the most difficult of consultations. It helps us guide and support patients through the RTP process, from acute pain management strategies right through the frustrations of lengthy rehabilitation. But unchecked, is it possible that our past experience, masquerading as empathy, can become a destructive entity that steps on the toes of evidence-based sports medicine?
I recently saw a long-suffering patient in clinic with knee ‘locking’, who’d had referral for surgery deferred for years by a doctor with a sporting interest. It emerged that this well-meaning doctor had experienced a bad outcome from meniscal debridement, at the same age that his patient had presented. Yet it is commonly acknowledged that these knee symptoms respond well to arthroscopic intervention. Any clinician in any specialty can get too involved with guiding the patient to the correct decision, yet in SEM the odds on this happening may be higher because of our innate passion for sport.
How should we deal with this phenomenon? Just as we can learn to recognize frustration, anger or exasperation in a consultation and to emotionally ‘house-keep’, it is equally important to maintain spectatorship with regard to the impact of our personal past experience. Reading a patient’s notes or hearing the presenting complaint should set alarm bells ringing and provide the mental cue. We should be prepared to take stock and step back to consider our views and their potential consequences. For whilst our experiences in sport may make us better SEM clinicians, fit to stand on our evidence-based soapboxes, we may inadvertently be practicing hypocrisy by preventing our patients getting the treatment both that they deserve and that research demands.
***************************************************************
Dr James Noake is a Sport and Exercise Medicine trainee currently placed at Charing Cross Hospital, London. He is team doctor for London Irish RFC, works as a medical officer for England / GB Disability Football and is clinical lead in orthopaedics, SEM and musculoskeletal medicine for Herts Valleys Clinical Commissioning Group (HVCCG)”
Dr James Thing co-ordinates “Sport and Exercise Medicine: The UK trainee perspective” — a twice-monthly blog
BJSM welcomes guest blogs from the 8 national member society groups as well as from others.