Inspired by Wang et al Acupunct Med 2017[1]
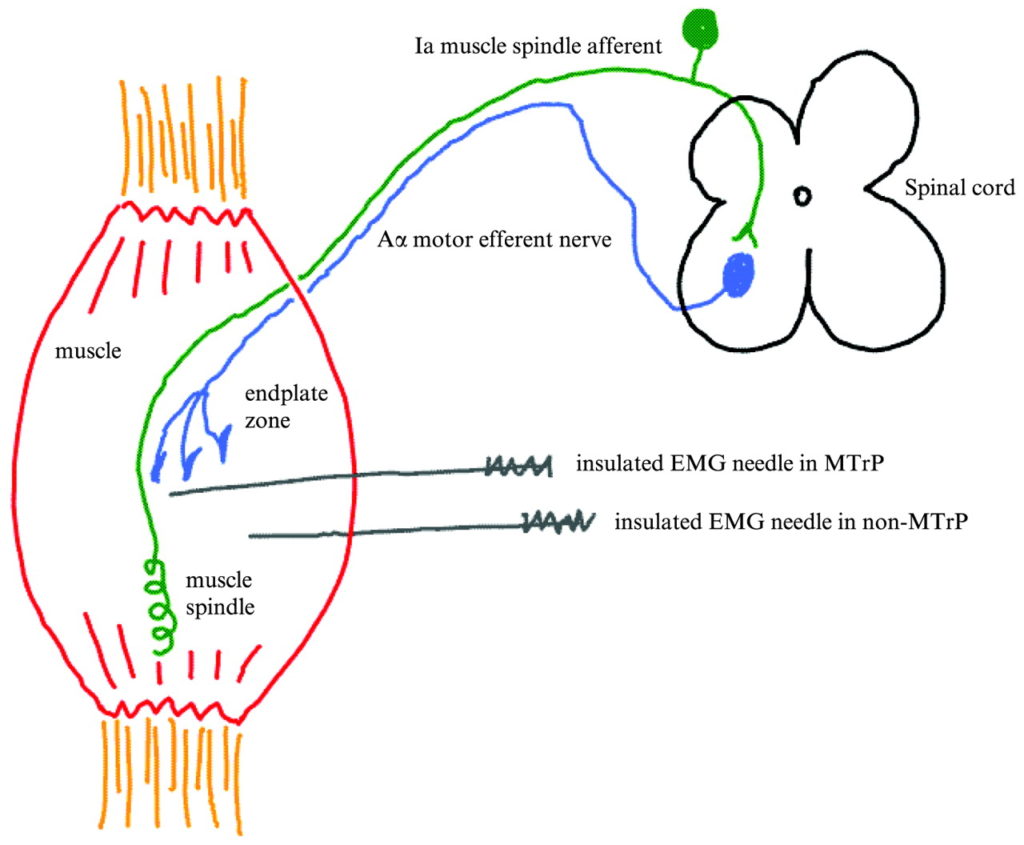
Image taken from Cummings M Acupunct Med 2009.[2]
I got interested in swapping my hypodermic needles for filiform ones some 25 years ago, and was encouraged by my early success treating myofascial pain in a military population.[3] I became more and more expert at identifying these targets we call trigger points, touching them briskly with the tip of my fine filiform needle, and seeing them twitch with almost immediate relief of pain and tightness in the muscle. The twitch seemed to go along with immediate results, but it could be elusive, and other colleagues claimed similar success with less 3 dimensional accuracy – superficial needling or simply needling an acupuncture point nearby. As I have followed the clinical research in acupuncture I became less and less convinced that my accuracy, and the accuracy I tried to teach would be validated since there was so little difference between even real and sham needling.
My early research was a review of all both wet and dry needling in myofascial pain.[4] There was a strong suggestion that when injecting trigger points (wet needling), the substance in the syringe did not seem to matter, but all groups appeared to improve dramatically. At the time there were not many trials using filiform needles.
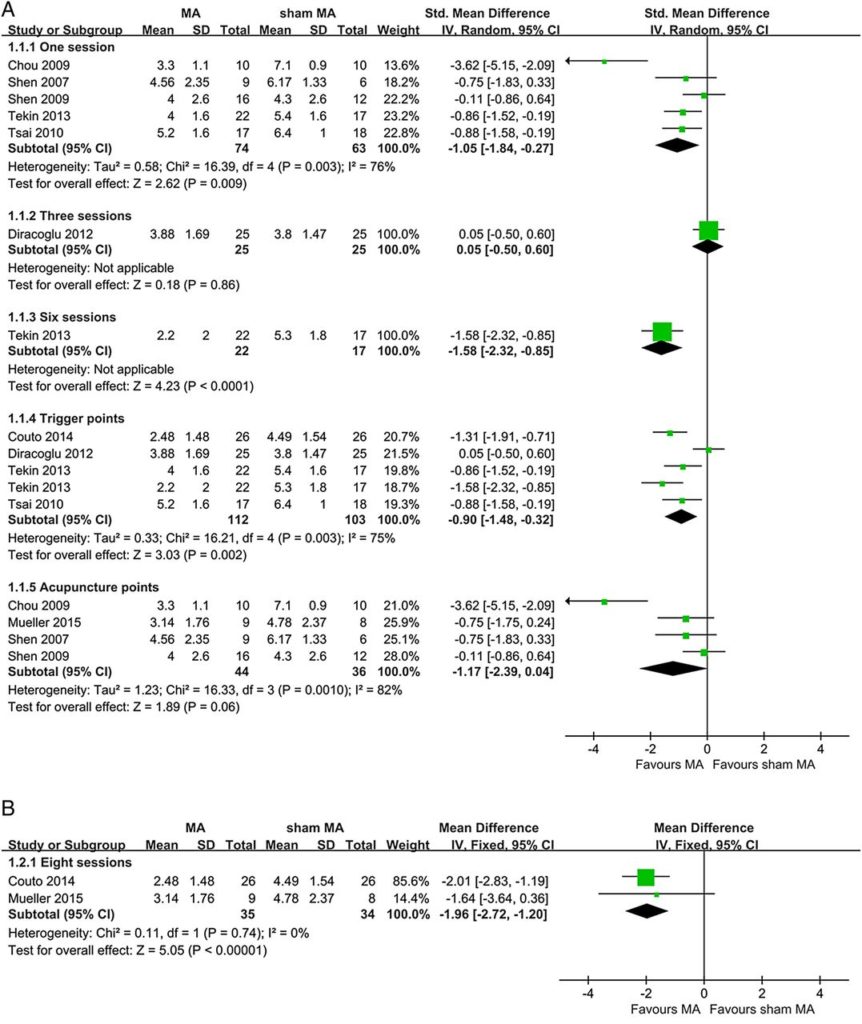
Now we have a selection of trials that can be combined in meta-analysis, and the tentative conclusion is that targeting trigger points seems to have some specific effect over sham, but that targeting acupuncture points is not clearly superior to sham.[1]
Figure 3 from Wang et al Acupunct Med 2017[1]
It is always worth having a careful look at Forest plots – so easy to miss the wood for the trees, so to speak, or even overlook some very strange trees! There are some issues to note here. The results of one trial (1.1.4 Tekin 2013) got included twice, albeit at different time points – they probably should have just decided on using one time point. Then there is a noticeable outlier in the lower plot (1.1.5 Chou 2009) – the effect size of this trial was huge in comparison to all the others. Under these circumstances it is always worth doing a sensitivity analysis excluding outliers. In this case it led me to check the original paper, and whilst the authors of this review classified it under acupuncture point treatment rather than trigger point treatment, the paper seems to suggest it used a trigger point needling technique to obtain multiple local twitch responses (LTRs) from remote trigger points that happened to be also at acupuncture point sites – in this case LI11 & TE5. Tricky to know how to classify this one then, but wait, there is another paper that used remote needling of a trigger point and measured an effect on upper trapezius myofascial pain (1.1.4 Tsai 2010). Maybe we should exclude that one as well in sensitivity analysis? Well I would have done all that for you, but given the small total number of total participants and the risk of bias, any conclusions would be unlikely to rise beyond a tentative suggestion.
So there you have it, perhaps the first meta-analysis of filiform needling in myofascial pain that points towards more accurate targeting of trigger points – but we have a long way to go!
References
1. Wang R, Li X, Zhou S, et al. Manual acupuncture for myofascial pain syndrome: a systematic review and meta-analysis. Acupunct Med 2017. doi:10.1136/acupmed-2016-011176
2. Cummings M. Myofascial trigger points: does recent research gives new insights into the pathophysiology? Acupunct Med 2009;27:148–9. doi:10.1136/aim.2009.001289
3. Cummings TM. A computerised audit of acupuncture in two populations: civilian and forces. Acupunct Med 1996;14:37–9. doi:10.1136/aim.14.1.37
4. Cummings TM, White AR. Needling therapies in the management of myofascial trigger point pain: a systematic review. Arch Phys Med Rehabil 2001;82:986–92. doi:10.1053/apmr.2001.24023
Declaration of interests
I am the salaried medical director of the British Medical Acupuncture Society (BMAS), a membership organisation and charity established to stimulate and promote the use and scientific understanding of acupuncture as part of the practice of medicine for the public benefit.
I am an associate editor for Acupuncture in Medicine.
I have a very modest private income from lecturing outside the UK, royalties from textbooks and a partnership teaching veterinary surgeons in Western veterinary acupuncture. I have no private income from clinical practice in acupuncture. My income is not directly affected by whether or not I recommend the intervention to patients or colleagues, or by whether or not it is recommended in national guidelines.
I have not chaired any NICE guideline development group with undeclared private income directly associated with the interventions under discussion. I have participated in a NICE GDG as an expert advisor discussing acupuncture.
I have used Western medical acupuncture in clinical practice following a chance observation as a medical officer in the Royal Air Force in 1989. My opinions are formed by data that spans the range of quality and reliability, much of which is in the public domain.
I have a logical mistrust of the motives of anyone who advertises an interest or hobby in being a ‘Skeptic’, as opposed to using appropriate scepticism within their primary profession, or indeed organisations that claim to promote generic ‘science’ as opposed to actually engaging in it.