Modern medicine is advancing at an eye-watering pace, and treatments are being utilised for ever-widening patient groups, who might not have been offered similar therapies even a few short years ago. In this context, it is increasingly important to know that these remarkably effective, expensive, and life-changing treatments are aligned with the wishes of our patients.
Renal medicine is just such an area where a once relatively rare treatment, offered to relatively few patients (HD) is now being offered to an expanding pool of patients. In a paper in last month’s PMJ, Davison and Sheerin describe some of the challenges around the provision of HD to patients with CKD.
There can be no doubt that HD makes a huge difference to patients with CKD who require it – both positive and negative. However, it was surprising to read that some studies have found up to 60% of patients on HD regretted the decision. Sadly it was less surprising to see that a number of these patients felt that either their families or their physicians played a role in ‘pressuring’ patients to embark on this treatment.
Doctors train for many years to be able to manage diseases, put off the inevitable, and maintain the functioning of vital organs through acute and chronic illness. As such it is entirely understandable that they would wish to offer treatments they have at their disposal to their patients, especially where these treatments can confer a survival advantage. However, the doctors involved in these decisions may not be best placed to ensure that these treatments are initiated for the correct reasons… and it is a feature of many consultations I have had with patients over the years that they often take actions to please their relatives – even if their own preference might be something else entirely.
As we enter the sunset of the baby boom generation, and we develop ever more effective treatments to treat once terminal illnesses, the medical profession must start to take the idea of patient preference more seriously. This is especially so where resources are scarce, and making the wrong diagnosis of patient preference can lead to (potentially) years of treatments which the patient may well regret starting in the first place, or to missed opportunities to intervene when assumptions have been made in the opposite direction.
There are two key steps that we must make to move towards true patient choice.
One is by enhancing our skills at sharing decision making with our patients and for specialist services to start developing relationships with patients that allow a better understanding of their hopes, concerns and expectations for the future. As Iona Heath pointed out in her fantastic Harveian Oration in 2011 – GPs tend to deal with one set of patients, but their illnesses change over time, but specialists tend to deal with fewer diseases, but it is the patients that come and go. As such, specialists will be on the back foot when it comes to developing a deep understanding of the true wishes of their patients, but with time, care and with the right tools it is possible to get nearer to the ideal scenario for our patients.
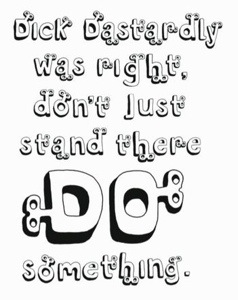
The other is to realise that just because we can do something, doesn’t mean that we should. This last issue may take a little longer to resolve. Diane Plamping highlighted this ‘can do, should do, and that doing means treatment’ thinking as a central tenet of working in the NHS in an article for the 50th anniversary of the organisation. She offered no quick fix, but does encourage us to talk about ‘can do, should do’ with our colleagues. I would suggest that we should discuss this with our patients. For those we have known for a long time, we will be halfway towards knowing their true preferences, for those who we have met more recently, we need to afford a little more time to ensure that we make perhaps the most important diagnosis when it comes to long-term conditions – the patient’s preference.