Poor communication is often at the root of complaints about clinical care (see here and here)
Poor communication with patients is concentrated on in a number of spheres of medical education – the CSA exam from the Royal College of General Practitioners is an example where consultation style and communication is assessed as a key outcome for career progression. Medical schools deliver communication skills training, and postgraduate training (especially for General Practitioners) sets a premium on communication between healthcare professionals and their patients.
In the background is communication between healthcare professionals within a team, or on different teams. Acute situations are often covered well, and the ALS training system is a good example of creating a common language which enables swift understanding and communication in a time critical situation. Work within simulation labs in particular is bringing communication tools from other industries to bear on emergencies, and ‘crisis resource management‘ – with an emphasis on team communication is very much part of the current vogue in anaesthetic training (among other specialties)
But what about that staple of the medical world – the notes? Are we all trained as well in communicating in the written form?
As electronic notes loom on the horizon, perhaps it is understandable that note writing is becoming a lost art, and flourishes with a fountain pen becoming a rarity.
However, until we reach the nirvana (?) of a fully electronic patient record, we still have the task of communicating the complexities of a clinical examination in the notes.
An organ close to my (and your) hearts – is the lungs. Examination of the lungs with a stethoscope has fallen out of favour in some quarters but remains a key procedure in investigating the acutely unwell, or recuperating patient.
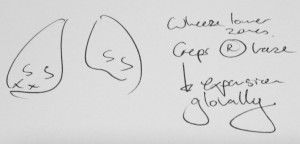
In the PMJ this month is a great paper on the use of different symbols used in medical notes to ‘describe’ findings in the chest examination – and the conclusions make a lot of sense. I was surprised to see foreign symbols which would make no sense to me at all, but reassured by the simple advice to make these hieroglyphics more understandable. Below is one of my standard examination pictograms. I seem to have a different dialect from the studied population for wheeze, but agree with them in general for crackles…
A common language would be the ideal, and this paper shows how we can improve this small but vital part of our communication in the notes.
When thinking about how to tackle this on a wider scale, it is tempting to think that to improve the accuracy, relevance and quality of note-making, the most senior member of the team during that consultation makes the note. This is not the usual experience on ward rounds – where the most junior member of the team often scribbles down their interpretation of a consultation and then defines the actions taken by the team thereafter.
To enhance educational opportunities on the ward round, improve team understanding of the case, and the patient’s understanding of what is happening to them, Dr Caldwell in Worthing uses a technique which is discussed on this thread
The PMJ paper sets out the variation possible in understanding a ‘set-piece’ of clinical examination when written in the notes; we need to take the lessons from this and apply them more widely – to improve communication – which will in turn enhance patient safety, and potentially experience and engagement too.