Dr Helen Noble, Lecturer & Clare Carswell, Undergraduate mental health nursing student, Queens University Belfast
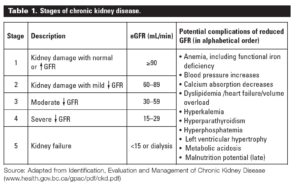
There are at least 59,000 adult patients receiving renal replacement therapy to treat end stage kidney disease (ESKD) in the United Kingdom. In addition there are over 1.8 million people being treated globally – 77% treated with chronic dialysis and 23% living with a transplant. Kidney disease is categorised into five stages depending on the estimated glomerular filtration rate and evidence of kidney damage. The most severe of these stages is stage 5 Chronic Kidney Disease where the eGFR is < 15 ml/minute/1.73m (table 1).
The number of older patients with ESKD is increasing annually as the population ages. The UK population aged over 65 is predicted to increase by 60%, from 10.3 to 16.9 million by 2035 [https://esa.un.org/unpd/wpp/], and increased numbers of older patients will commence dialysis worldwide. Older patients who require dialysis report a higher burden of “geriatric syndromes”. These include frailty, falls, and cognitive impairment. There is also evidence that dialysis initiation may be associated with accelerated rates of functional and/or cognitive decline [https://www.ncbi.nlm.nih.gov/pubmed/15507063]
Renal replacement therapy includes haemodialysis, peritoneal dialysis or transplantation but choices regarding treatment are perplexing. One particularly difficult decision concerns older people with ESKD, unsuitable for transplantation, who have to decide between dialysis and conservative management. Dialysis involves coming to hospital three times a week for four hours each visit and requires attachment to a dialysis machine which filters the blood and replaces the role of the damaged kidneys. Conservative management offers a supportive and palliative approach to care, without dialysis. Patients are supported and followed up by a multidisciplinary team often in their own homes. Some people regret their decision to start dialysis and some may go on to withdraw from treatment. Others report that they didn’t fully understand the decision they were making. There is a need to ensure that patients making decisions between dialysis and conservative management are supported through this process. Decision-aids may help people who are facing these difficult health treatment decisions. Decision-support interventions encourage people to be more actively involved in decision making, improve risk perceptions and congruence between the choice made and their personal values. They may also help improve communication between patients and staff.
There are limited decision-support interventions available to assist with complex decision-making in people who are choosing between dialysis and conservative management. The OPTIONS decision-aid has been developed in Australia and is being tested in a multisite randomized controlled trial [http://www.readcube.com/articles/10.1111/jan.12921]. A similar tool is being developed in Ottawa, Canada. In the UK, The excellent ‘Dialysis Decision Aid’ has been developed to help people make decisions about renal replacement therapy but it has less of a focus on conservative management and is aimed at all age groups [https://www.kidneyresearchuk.org/DialysisDecisionAid].
In the UK there is a need to develop a UK specific decision-aid for people deciding between dialysis and conservative management in order help patients with kidney disease make the best possible decision. In order to test such an aid a randomised trial similar to the one in Australia is recommended.