The LIFE study (Lifestyle Interventions and Independence for Elders) is a multicenter study to assess the effects of physical activity in prevention of major mobility disabilities in older adults (see DOI:10.1001/jama.2014.5616).
Background: Mobility (ability to walk without assistance) is important for independent functioning and is inversely related to morbidity, disability and mortality.
Results: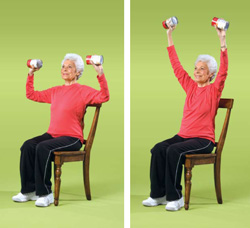
— 1635 sedentary men and women 70-89 yo (mean 79), average BMI of 30, 74% White, 20% African-American, 4% Latino, with physical limitations but were able to walk 400 m, were randomized to structured moderate-intensity physical activity (2 center-based visits/week and home-based activity 3-4 times/week with goal of 150 min/week walking, and strength, flexibility, and balance training) or health education program (weekly workshops of health education during the first 26 weeks and then monthly, focusing on prevention, screening, negotiating the healthcare system, but NOT physical activity). Participants recruited from the community. They were followed for 2.6 years.
–Primary outcome: Major mobility disability, defined as inability to complete a 400-m walk test within 15 minutes without sitting or help from another person or a walker, though they could stop up to 1 minute for fatigue.
–The physical activity group attended 63% of scheduled sessions, excluding medical leave (59% had medical leave at least once)
–Physical activity group increased activity by 138 minutes per week to 218 min/week. Health education group increased 34 minutes to 115 min/week
–The difference was 40 min/week for moderate physical activity, as assessed by accelerometry, throughout the followup period
–Persistent mobility disability (defined as 2 consecutive major mobility disability determinations) in 120 of those in physical activity group (14.7%) vs 162 in the health ed group (19.8%), with HR of 0.72 (0.57-0.91)
–Major mobility disability or death in 264 (32%) of physical activity group and 309 (38%) in health ed group, with HR 0.82 (0.70-0.97)
–The subgroup with lower physical function at baseline (Short Physical Performance Battery <8) had the most benefit in terms of major mobility disability (HR=0.75). No difference if stratify post-hoc by cognitive ability.
–No difference in safety/adverse events between the groups, though should be pointed out that physical activity group non-significantly trended to having more serious events (if exercise does unmask subclinical heart failure, etc)
–Cost of intervention was $4900/participant over 2.6 years.
So, though did rely on self-reported activities, this was a pretty impressive RCT in that a not-so-expensive intervention begun in already mobility-impaired elderly for only 2.6 years (though average life-expectancy was 9 years) significantly decreased development of major mobility disability. Though no evident benefit on clinical outcomes in this short-term study in mobility-impaired elderly, this study confirms data on younger people and those without pre-existing mobility limitations (ie, there seem to be benefits for pretty much everyone). Exercise does improve several important physiologic effects, including improved lipids (increase HDL, decrease LDL), and decrease in CRP, fibrinogen, blood viscosity, plasminogen activator inhibitor-1, platelet aggresation/adhesion, blood pressure, diabetes, osteoporosis, obestiy, colon and breast cancer, anxiety, depression, functional decline, falls/functional limitations, cardiovascular disease and stroke…..
In addition, another recent study in people over 65 found that exercise also decrease heart rate variability, an assessment of autonomic function and in several studies found to be associated with risk of heart disease (see DOI:10.1161/CIRCULATIONAHA.113.005361). In this 5-year study, 985 people in the Cardiovascular Health Study (mean age 71, 40% male, 66% White, 36% with > high school education, 10% smokers, resting heart rate of 67, 45% with htn, 16% diabetes), looking at amount of physical activity (observational study) and heart rate variability by 24-hour Holter monitor (done at baseline at at 5 years).
Results:
–Greater leisure-time activity, walking distance, and walking pace were each associated prospectively with an array of measured more favorable indices of heart rate variability, both in those with the highest reported physical activity and in those whose physical activity increased over time.
So, this study in the elderly confirms others in younger patients, that physical activity (perhaps modulated through reduced sympathetic activity) results in less heart rate variability, which might be an additional mechanism for the positive clinical effect of exercise.
Geoff